What is Age-Related Macular Degeneration?
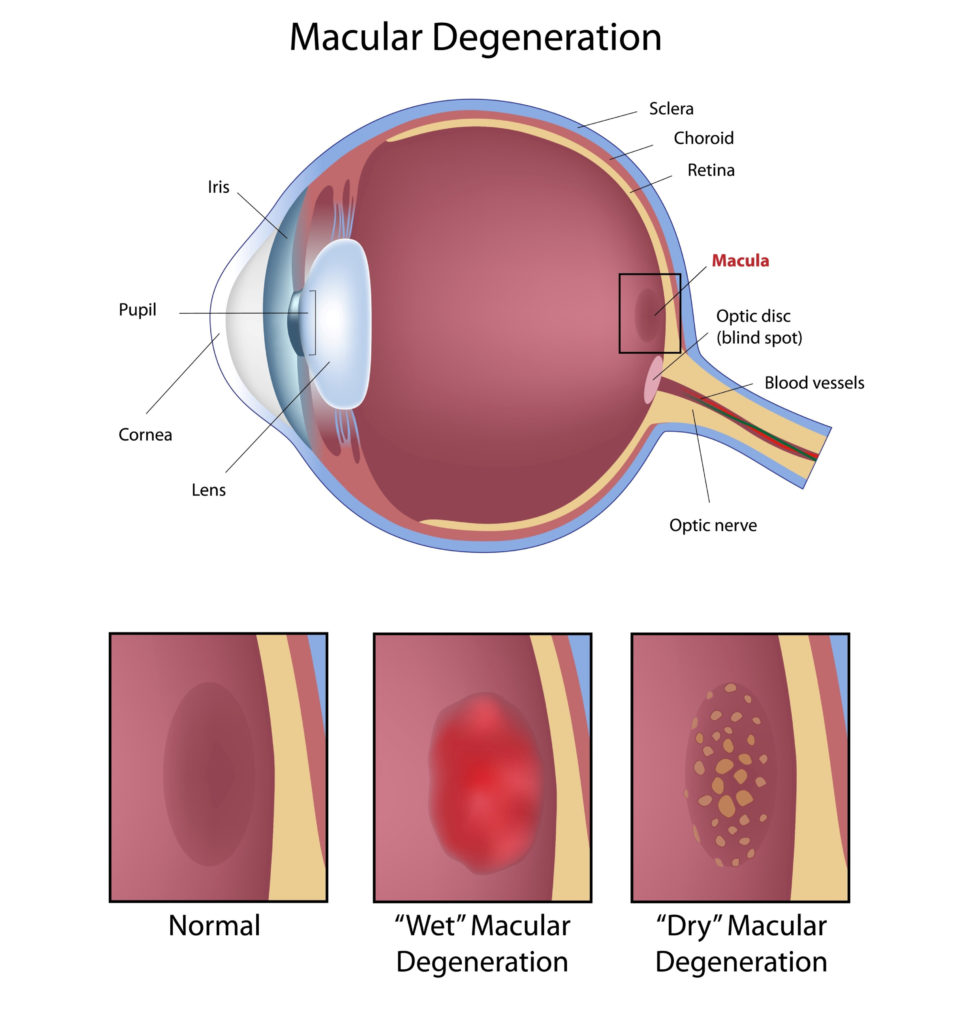
Age-related macular degeneration, sometimes referred to simply as macular degeneration or AMD, happens when the macula degrades and affects your vision. Like many eye diseases, it’s most common in people over age 50, and it’s the leading cause of blindness in industrialized countries like Canada.
Dry AMD vs. Wet AMD
There are 2 types of AMD: dry AMD and wet AMD.
Dry AMD
The dry form of AMD is the more common and less severe type. 90% of people with AMD have dry AMD. Dry AMD happens when there is deterioration of the deeper layers of the retina, specifically in the macula. Drusen (clumps of protein) can develop as well as changes in the retinal pigment layer.
As dry AMD progresses, it causes gradual loss of central vision. Dry AMD can also sometimes advance to wet AMD. In many cases, patients with dry AMD can still have very good central vision. There can be a range in the severity of vision loss caused by AMD, which is why it’s important to have the condition diagnosed by an optometrist.
Wet AMD
Wet AMD is the more devastating form of AMD, causing quicker and more substantial vision loss. Only 10% of people with AMD have wet AMD, but it accounts for 90% of blindness caused by AMD.
Wet AMD can result in the growth of abnormal blood vessels in the choroid (the vascular layer of the eye). As fluid leaks from these abnormal blood vessels, damage to the deep layers of the retina may occur and result in rapid vision loss.
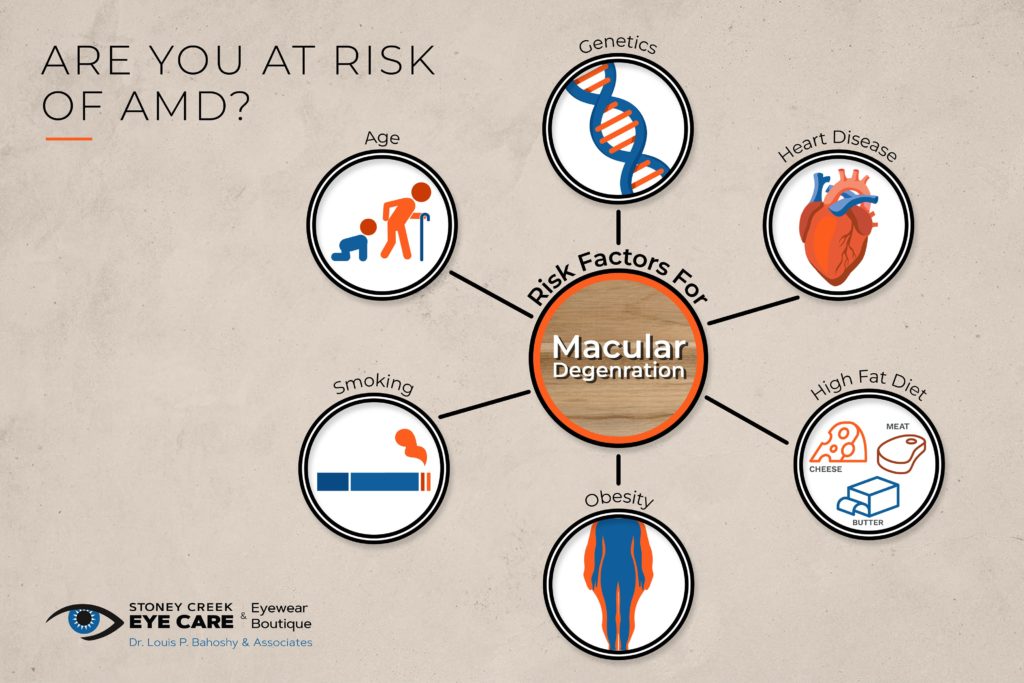
Risk Factors
AMD is more common in people who are:
- Over the age 50
- Smokers
- Overweight
- Caucasian (white)
Other risk factors include:
- A diet high in saturated fat (butter, meat, cheese)
- Hypertension (high blood pressure)
- Heart disease
- High cholesterol
- A family history of AMD
Symptoms
You could have AMD if you have:
- Difficulty reading
- Difficulty driving (especially at night)
- Trouble recognizing facial features
- Blurry, distorted, or blank spots in your vision
- Can be identified with an Amsler Grid
Any changes in your vision should be addressed by your optometrist immediately. They can help diagnose AMD and other issues that could be causing your vision loss.
Diagnosis
It’s important to diagnose AMD as soon as possible, so you can begin treatment and prevent further damage to your vision. Most diagnostic tools used for AMD involve looking at the retina to identify any abnormalities caused by AMD.
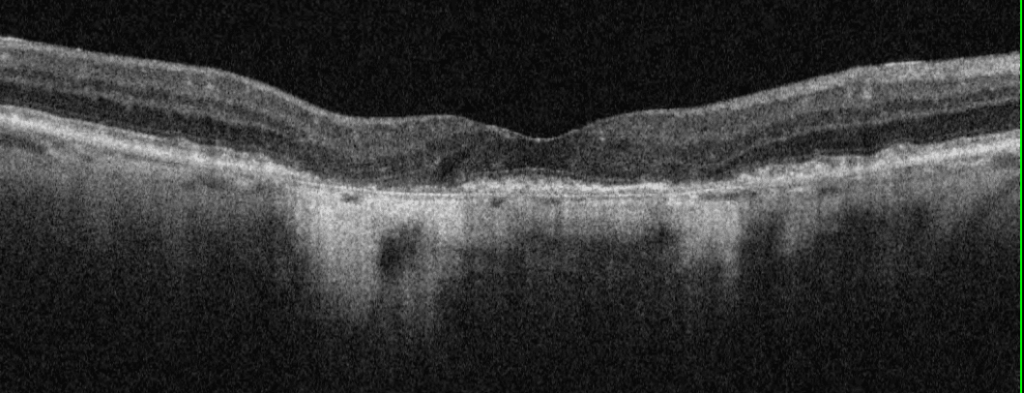
Optical Coherence Tomography
Optical coherence tomography (OCT) gives your optometrist a detailed photo of your retina. An OCT image shows the distinct layers of the retina, helping to identify AMD.
OCT angiography can also be used to identify the choroidal neovascular membranes in wet AMD. It’s a less invasive alternative to fluorescein angiography, and no dye is needed.
Digital Retinal Images
Digital retinal images also help give a detailed look into the retina and macula. These images can show drusen, blood, or lipids resulting from wet AMD. They can also identify areas of scar tissue and atrophy (areas where the retinal cells have wasted away and died.)
Dark Adaptation Testing
Dark adaptation testing measures how well your eyes adjust to the dark and how sensitive your eyes are in the dark. During the test, you’ll look into a specialized instrument and your optometrist will determine how well your retina responds to low light conditions after being exposed to a bright light.
The earliest signs of AMD can include problems with dark adaptation. AMD patients typically take longer to adjust to changes in light, especially going from bright to dark environments. This is why night driving is often challenging for AMD patients.
Genetic Testing for AMD
Genetic testing for AMD helps determine your risk of developing AMD and the right treatment if you have the disease. The test is non-invasive and simply requires a cheek swab (a Q-tip is gently rubbed across the inside of your cheek to collect a DNA sample).
Genetic testing is easy and painless, although there is some debate in the scientific community about whether it is necessary. Some believe that it provides valuable insight, whereas others believe there isn’t enough evidence to justify genetic testing.
Understanding of AMD continues to evolve, and with it, so will the role of genetic testing. Right now, many believe that genetic testing can provide insight into AMD treatment, particularly for no zinc or low zinc treatments.
No Zinc vs. Low Zinc Treatments
Research is still emerging, but the current evidence suggests that some patients require different levels of zinc when treating AMD. Some people benefit from zinc, whereas for others, zinc can actually increase their likelihood of developing AMD. Studies continue, but for now, genetic testing can help inform the best nutritional supplements for you.
Dry AMD Treatments
There is no direct treatment for dry AMD. However, dry AMD can be managed with nutrients, supplements, and lifestyle changes.
AREDS & AREDS 2 Supplements
The AREDS studies were comprehensive studies designed to measure how nutritional supplements affect the progression of AMD. The original AREDS study concluded that high levels of certain nutrients, including vitamins, antioxidants, and minerals, can reduce advanced AMD by about 25%. The AREDS 2 study found that AMD patients can also benefit from macular carotenoids (lutein and zeaxanthin).
| Nutrient | AREDS Formula | AREDS2 Formula |
| Vitamin C | 400 mg | 400 mg |
| Vitamin E | 400 IU | 400 IU |
| Beta-carotene | 15 mg | – |
| Copper (cupric oxide) | 2 mg | 2 mg |
| Lutein | – | 10 mg |
| Zeaxanthin | – | 2 mg |
| Zinc | 80 mg | 80 mg |
Macular Carotenoids
Macular carotenoids are the pigments found in the macula, which are essential for vision clarity and protection. You can get these nutrients in certain foods, like kale, spinach, bell peppers, and salmon and in supplements.
The 3 macular carotenoids are lutein, zeaxanthin and meso-zeaxanthin. They are responsible for filtering harmful blue light and neutralizing free radicals. Supplements containing all 3 carotenoids increase the macular pigment optical density (MPOD) of your eye. By increasing MPOD, macular carotenoids can help protect the macula and potentially improve visual function and contrast sensitivity. The AREDS 2 study recommends lutein and zeaxanthin, although science now favours supplements with all 3 macular carotenoids: lutein, zeaxanthin, and meso-zeaxanthin.
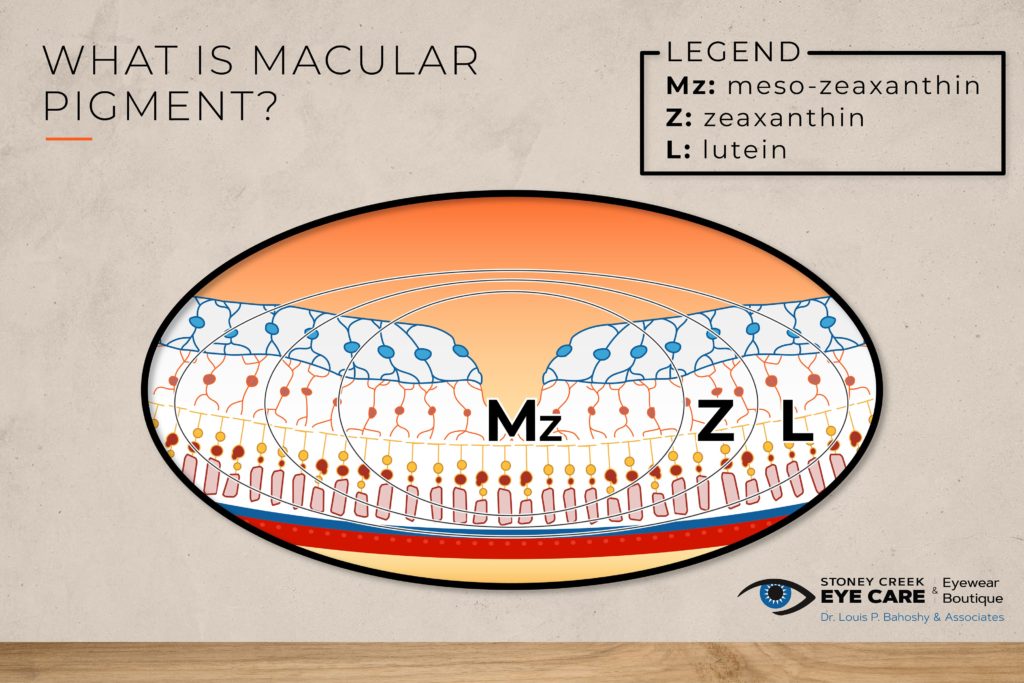
In early to moderate AMD, the current evidence shows that a supplement containing lutein, zeaxanthin, and meso-zeaxanthin is the best option. Macuhealth and Vision Essence Early Defence are 2 supplements that contain all 3 macular carotenoids in the appropriate amounts.
An AREDS 2 type formulation has not been shown to be beneficial for early or mild cases of AMD. Instead, a modified AREDS 2 type formulation, with low zinc (25 mg) or no zinc depending on the advice of your optometrist is reserved for more moderate to advanced cases of AMD.
Lifestyle Changes
In addition to supplements, certain lifestyle changes can reduce the risk and progression of AMD. Obesity, hypertension, and smoking are significant risk factors. By changing your lifestyle through weight loss and quitting smoking, you can help lower your risk of AMD. Limiting UV exposure can also help reduce your risk. When you do go outside, always make sure you’re wearing sunglasses to protect your eyes.
Wet AMD Treatments
Anti-VEGF Injections
For wet AMD, the most common and effective treatment is anti-VEGF injections. Historically, treatments for AMD included laser treatments and photodynamic therapy, but today, anti-VEGF treatment is the gold standard.
VEGF is a healthy molecule that supports the growth of new blood vessels. Because wet AMD is caused by the growth of new, abnormal blood vessels, anti-VEGF injections can help slow the progression of wet AMD.Regardless of the type or severity of your AMD, the best chance of saving your sight comes with early diagnosis. Make sure you visit your optometrist for regular eye exams, especially if you’re over 50 or you have an increased risk of AMD.